- Are pregnant women more susceptible to infection or at increased risk for severe illness, morbidity, or mortality with COVID-19?
Although pregnant women have been more likely to become infected or severely ill from past outbreaks of other related coronavirus infections (SARS-CoV, MERS-CoV) as well as influenza, the limited data from China does not show a greater risk for of COVID-19 in pregnant women compared to other adults. The situation may change as more cases are identified but for now there is no special precautions for pregnant women beyond usual infection prevention measures. Follow the directions of your health care provider.
- Can a fetus be infected if a pregnant woman gets the virus?
There have only been a small number of cases in pregnant women so far but to date there is no evidence for intrauterine infection among women diagnosed with COVID-19 in the third trimester. There have also been a small number of cases of infants born to mothers with COVID-19 and none of these have tested positive. Also COVID-19 virus was not detected in samples of amniotic fluid. Newborns can get COVID-19 from adults and other people in their environment. Adults with possible or confirmed infection who are caring for newborn infants should follow CDC guidance, including with regard to breast feeding.
- I am pregnant patient and I work in a hospital setting, should I not care for patients that are potentially infected with COVID-19?
Pregnant healthcare personnel should follow best hand hygiene practice, universal precautions, and be aware of all updated infection control guidelines for their health care facilities to keep themselves and others safe in the healthcare environment. Your facility should have guidance for you to follow.

- I am planning international travel this spring/summer. Should I cancel?
The impact of COVID-19 around the world is changing quickly. All patients should avoid travel to areas designated with a Level 3 CDC Travel warning. Also consider in your travel plans not only the risk for infection but the availability of health care facilities if you need medical assistance. For pregnant patients, all international travel is strongly discouraged at the current time.
- I am planning domestic travel this spring/summer. Should I cancel?
The number of cases and locations of COVID-19 infection in the United States is changing rapidly. In this changing landscape, strongly consider whether your travel is essential. Be aware that you could be subject to significant travel restrictions, disruptions, and an inability to return to home should inadvertent exposure to COVID-19 occur. Talk to your health care provider if you have additional risks in addition to pregnancy. Pregnant women at particularly high risk such as those with pulmonary co-morbidities or immunosuppression should avoid all travel. Review the latest information and advisories before embarking on any trip.
6. I was near a person recently who was coughing. What should I do? Should I be tested?
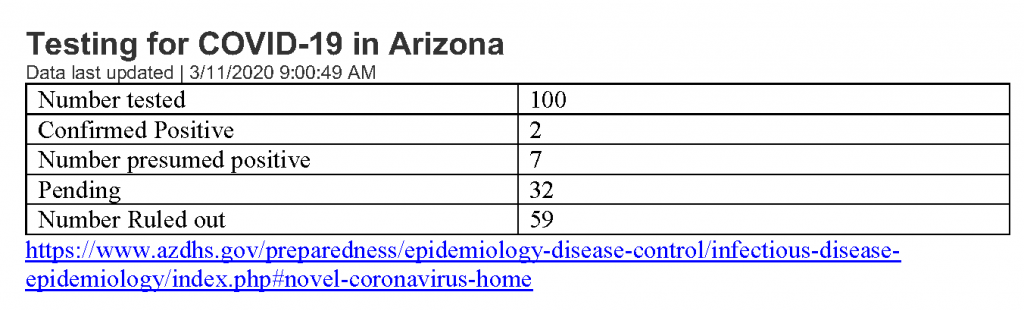
No testing is indicated in this situation. The COVID-19 tests are currently only used for patients with symptoms and/or risk factors such as travel to Level 3 areas or exposure someone who has been confirmed positive for COVID-19. Testing guidance is likely to change as tests become more widely available. Please refer to the AZ Department of Health for more information.
- I am concerned about going to crowded places. What should I do?
The CDC recommends that people with risk factors for severe disease (older adults and those with chronic medical conditions) spend most of their time at home and avoid activities that involve large crowds. Right now the CDC does not consider pregnancy alone to be a risk factor for increased disease severity but please talk to your obstetrician to make sure you don’t have other risk factors. Also if you live with someone in a high risk condition, you too will want to avoid exposure so you don’t infect that person. As always, practice good hand hygiene, and avoid touching your face.
8. I may have been exposed to someone with COVID-19, but I don’t have any symptoms myself. What should I do?
The Department of Public Health may want to track your patient (and potentially quarantine her) if she was in close contact with a patient with confirmed COVID-19. Please contact the Biothreats MD at your institution for further guidance.
9. I have a fever, cough, muscle aches, sore throat, and headache and I have traveled recently? What should I do? travel or community exposure.
If you have mild symptoms, call your health care provider before going in to the office. For severe symptoms like shortness of breath, high fever or feeling severely ill, you need immediate evaluation and testing. Wear a mask that completely covers your mouth and nose when you leave our home. Keep your mask in place and avoid touching the mask or your face until you are directed otherwise by a health care provider.
- I have a fever, cough, muscle aches, sore throat, and headache. I have not had any travel or exposure to COVID-19. What should I do?
You are much more likely to have the common cold or influenza (flu). These infections are much more common than COVID-19 at the moment. If you have mild symptoms, call your health care provider before going in to the office. For severe symptoms like shortness of breath, high fever or feeling severely ill, you need immediate evaluation and testing. If you have symptoms, always wear a mask that completely covers your mouth and nose when you leave your home. Keep your mask in place and avoid touching the mask or your face until you are directed otherwise by a health care provider